Spectra of pathogens predict lethality of blue light photo-inactivation
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Accepted: 24 April 2023
Authors
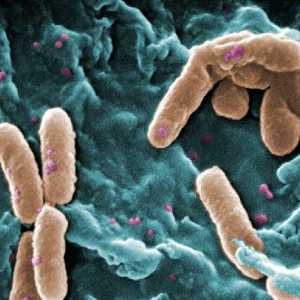
Whole-cell spectra of human pathogens are examined to identify species-specific wavelengths of maximum light absorption. It is presented how these data relate to clinical efficacy for antimicrobial phototherapies. Twelve species of microorganisms were cultured to exponential growth then processed and suspended in a scattering solution. Diffuse reflectance from the sample was delivered to two spectrometers that covered a spectral range of 370nm to 1200nm. Reflectance spectra were converted to relative absorbance. Absorbance spectra from multiple trials were averaged to produce a representative spectrum for each species. All pathogens studied demonstrated an absorbance spectrum with a primary component in the range 405-426 nm and 1-4 secondary components in the range 445-636 nm. Antibiotic-resistant and antibiotic-sensitive strains of Pseudomonas aeruginosa (Pa) had identical absorbance spectra. Whole-cell spectra support the hypothesis that a pathogen’s absorbance is directly related to efficacy of photoinactivation. The spectral signatures in all pigmented bacteria tested appear to be that of various combinations of in situ porphyrins. The knowledge of the absorption spectrum of a given pathogen provides a logical start for selecting the appropriate light source for a clinical trial.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






